Whether you're a clinician or a therapist, the SOAP note format offers a dependable method to track client progress and inform future treatment plans.
SOAP stands for Subjective, Objective, Assessment, and Plan. Each component plays a role in compiling a comprehensive client overview, making it easier to pick up where you left off in subsequent sessions or share critical details with other healthcare providers seamlessly.
Follow our comprehensive documentation series for templates and examples for all types of mental health clinical documentation like DAP notes, GIRP notes, BIRP notes, psychosocial assessment, biopsychosocial assessment, case conceptualization
How to Write SOAP Notes?
Let's understand each component of the SOAP note template:
Subjective (S)
The Subjective section captures the client's perspective and is the foundation of the SOAP note template. This includes their feelings, symptoms, and any personal concerns. Use the client's own words whenever possible to provide an authentic representation of their experiences. For instance, if a client says, “I've been feeling really anxious about work and haven't slept well in days,” these statements should be recorded here. The subjective data you collect might also include pertinent family history and details about present illness when applicable.
Objective (O)
In the Objective section, you document observable and measurable objective data. This might include physical exam findings, vital signs, medical history, and any notable behaviors observed during the session. This section acts as a counterbalance to the Subjective data by providing factual evidence. For example, you might note, “Client was tearful and avoided eye contact throughout the session.” This section should also document any temporal factors or aggravating factors the patient describes.
Assessment (A)
The Assessment section of the SOAP format is where you analyze the information gathered in the Subjective and Objective sections to provide a diagnosis or clinical impression. Here, you synthesize your observations with the client's reported experiences to determine the underlying issues. You might conclude, “Client exhibits symptoms consistent with Generalized Anxiety Disorder.” The assessment demonstrates your clinical reasoning and patient understanding based on subjective and objective information collected.
Plan (P)
The Plan section of the SOAP format outlines the next steps in the client's treatment. This could include immediate actions to be taken, long-term therapy goals, additional testing, and any follow-up appointments or specialist referral needed. Being specific in this section is crucial to provide clear direction for future physicians and other clinicians. For example, “Plan to start Cognitive Behavioral Therapy (CBT) focusing on anxiety management techniques. Next session scheduled for 10/20/2023.”
How long should your SOAP Note be?
When considering the length of your SOAP note, remember that quality is more important than quantity. Your goal is to present a clear and concise account of your session.
Typically, SOAP progress notes range from half a page to a full page, depending on the complexity of the session and the treatment being provided. Write soap notes that capture essential details without unnecessary elaboration.
Best practices in writing SOAP Notes
- Be Specific: Provide precise details relevant to the client's condition and progress.
- Stay Objective: Stick to observable facts and measurable data and avoid subjective interpretations outside the "S" section.
- Use Bullet Points: For lists within the Objective and Plan sections, use bullet points to enhance clarity and brevity.
- Review and Edit: Always review your notes for any redundant or extraneous information before finalizing.
By focusing on these best practices, you can ensure your SOAP notes are comprehensive yet succinct, making them effective tools in your therapeutic practice.
How to use AI to automate SOAP Notes
Tools like Supanote can now write notes automatically at the end of each session and completely automate your documentation. They're trained to write at the level of a PsyD, so it's like having your own PsyD assistant. What's more, some of them like Supanote can learn to write exactly like you.
How AI Therapy Note Tools Work
Most of these products typically work like this:
- Listen to session; you can just dictate your recollection after the session
- Generate full structured SOAP notes
- Maintain clinical accuracy and compliance standards
Below is a sample SOAP note written by Supanote.
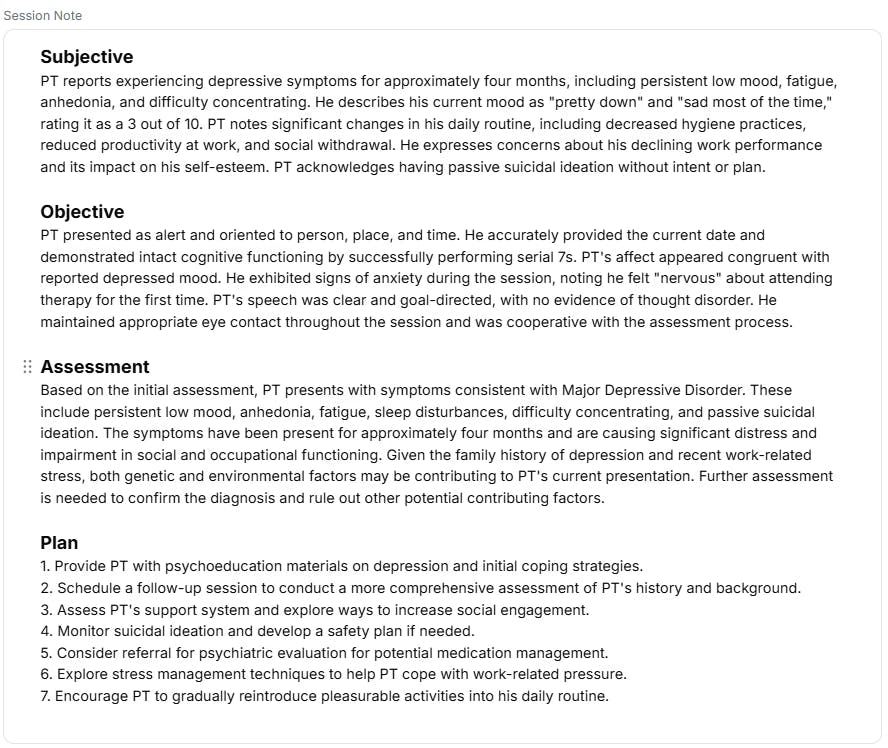
Supanote comes pre-built with several note templates, including SOAP, DAP, GIRP and many others.
You can directly sign-up for free and get started on Supanote here.
Save 4 Hours Every Week on Notes
Generate HIPAA-compliant drafts in seconds and focus more on your clients, not paperwork.
Start Free Trial
SOAP Note Templates and Examples
Below are several SOAP note template and examples across numerous use-cases. Use them to make your clinical documentation easier.
1. Individual Psychotherapy SOAP Note Example and Template
Let's say you're wrapping up a session with a client named Jane, who is dealing with anxiety. Here's how that could look:
Subjective (S): Jane reports feeling increasingly anxious over the past week, stating, "I can't shake this constant nervousness." She notes episodes of heart palpitations and difficulty sleeping, particularly before work meetings. Jane expresses concern over her performance at work and feels she might be on the verge of a panic attack.
Objective (O): Jane appeared visibly tense during the session, fidgeting with her hands and avoiding eye contact. Her speech was hurried, and she intermittently gazed at the clock. Notably, Jane's breathing was shallow, and she frequently sighed. Based on the GAD-7 scale, Jane scored in the moderate anxiety range.
Assessment (A): Jane's symptoms align with generalized anxiety disorder (GAD). The client shows signs of heightened stress related to work performance, suggesting a possible link between job-related tasks and her anxiety levels. Environmental triggers appear significant in contributing to her overall anxiety.
Plan (P): We'll focus on implementing relaxation techniques such as deep breathing and progressive muscle relaxation. Cognitive-behavioral strategies will be employed to address Jane's negative thought patterns associated with work performance. Plan to assess progress on these interventions in the next session. A follow-up appointment is scheduled for next week.
This example illustrates how a clear and concise SOAP note effectively captures important details of a therapy session.
2. Couple's Therapy SOAP Note Example and Template
The process of writing a SOAP note for couple's therapy might initially seem daunting, but it becomes more manageable once you get the hang of it.
Subjective (S): Both partners reported feeling disconnected and expressed frustration due to frequent arguments about financial management and household responsibilities. Partner A shared feelings of being overwhelmed and unsupported. Partner B disclosed concerns about financial insecurity and felt neglected.
Objective (O): Both partners displayed tense body language and had elevated tones during the session. Partner A frequently avoided eye contact, and Partner B demonstrated signs of anxiety, such as fidgeting and rapid speech. Both completed an introductory survey revealing moderate levels of relationship dissatisfaction on a standardized scale.
Assessment (A): The couple is experiencing significant relational tension, primarily driven by a lack of communication and unresolved financial stressors. The observed behavior and self-reported feelings suggest that both partners are struggling to voice their needs effectively. These issues contribute to a cycle of conflict, as evident from their interactions during the session.
Plan (P): Recommend starting weekly therapy sessions focusing on improving communication skills and addressing financial concerns. Assign homework to create a shared budget and schedule a check-in meeting later in the week. Introduce the concept of 'I' statements for more constructive dialogues. Reassess the couple's progress after four sessions to determine any necessary adjustments in therapy goals.
3. Family Therapy SOAP Note Example and Template
Family therapy presents unique dynamics and complexities, requiring clear and detailed documentation. Here's an example of how a family therapist might compose a SOAP note:
Subjective (S): The Martinez family attended the session today. The parents expressed concerns about their teenage daughter's recent withdrawal and declining academic performance. The daughter, Maria, mentioned feeling overwhelmed by school and family expectations. She expressed a desire to communicate more openly but feels judged.
Objective (O): The therapist observed Maria's body language, noting her crossed arms and minimal eye contact with her parents. Parents appeared visibly frustrated but attempted to engage in active listening. Family members became defensive at various points during the session, indicating a high level of tension.
Assessment (A): Maria is experiencing significant emotional distress due to perceived high expectations from her parents and academic pressures. Family communication patterns are contributing to misunderstandings and conflict. The current family dynamic is strained, with a clear need for improved communication and support strategies.
Plan (P): The therapist will employ a family systems approach to enhance communication and empathy within the family unit. Techniques such as active listening exercises and I-statements will be introduced in the next session. The therapist will also encourage setting realistic expectations and revisiting family goals to reduce pressure on Maria.
4. Group Therapy SOAP Note Example and Template
Group Therapy sessions are usually the hardest to document, but remember you just need to capture the highlights and interplay between the group. A good note could be as short as the one below.
Subjective (S): Several group members expressed feeling more connected and less isolated since joining the group. Jane mentioned that she found it helpful to hear stories of others going through similar struggles, which reduced her anxiety about her own situation.
Objective (O): The group engaged in a mindfulness exercise for 10 minutes. All members participated actively, with no signs of distraction. Physical markers such as relaxed postures and open body language were observed in participants.
Assessment (A): There is noticeable progress in terms of group cohesion and mutual support among participants. Jane's reduction in anxiety symptoms indicates that the group dynamic is positively influencing individual mental health.
Plan (P): Continue with mindfulness exercises and introduce cognitive-behavioral techniques to address individual issues more deeply. Plan for another round of personal sharing to reinforce group trust and cohesion.
5. Social Worker SOAP Note Template and Example
It's quite common to write soap notes in social work. SOAP notes by social workers follow a similar format, just the content varies, like less focus on elements like medical history, physical examination. Here's what a social work SOAP note typically looks like
S (Subjective): Client reports ongoing conflict with a neighbor regarding noise complaints, causing distress. States, "I'm feeling angry and frustrated. I can't relax in my own home." Reports difficulty sleeping due to anxiety about the situation.
O (Objective data): Client appeared agitated during the session, speaking rapidly and gesticulating frequently. Affect was congruent with reported mood. No signs of substance abuse or self-harm were observed.
A (Assessment): Client is experiencing significant stress due to environmental factors (neighbor conflict). This is impacting her sleep and overall well-being. Client demonstrates good insight into the problem but struggles with effective communication and conflict resolution skills.
P (Plan):
- Discuss and role-play conflict resolution strategies.
- Provide information on local mediation services for neighbor disputes.
- Refer client to community sleep hygiene workshop.
- Explore client's support system and coping mechanisms.
- Schedule follow-up appointment in two weeks to assess progress and adjust interventions as needed.
6. SOAP Note Example for Counselors
S (Subjective): Client reports feeling "overwhelmed" with work responsibilities. States, "I can't keep up with deadlines, and I'm constantly anxious about disappointing my boss." Mentions difficulty concentrating and occasional panic symptoms when thinking about work.
O (Objective): Client appeared tired, with slumped posture and dark circles under eyes. Speech was slightly pressured when discussing work situations. Completed GAD-7 with a score of 14, indicating moderate anxiety.
A (Assessment): Client presents with symptoms consistent with Generalized Anxiety Disorder, primarily focused on work-related stressors. There's evidence of negative self-talk and catastrophizing thoughts regarding job performance. Sleep appears to be impacted, potentially exacerbating anxiety symptoms.
P (Plan):
- Introduce cognitive restructuring techniques to address negative thought patterns.
- Teach and practice progressive muscle relaxation for anxiety management.
- Assign homework: thought record for work-related anxious thoughts.
- Discuss time management strategies for work tasks.
- Consider referral for psychiatric evaluation if anxiety symptoms persist or worsen.
- Next session scheduled for one week to monitor progress and continue CBT interventions.
7. SOAP Note Example for Psychiatrists
S (Subjective): Patient reports improvement in depressive symptoms since starting fluoxetine 20mg daily 4 weeks ago. States, "I have more energy and my mood is better." Sleep has improved but still experiences occasional early morning awakening. Denies suicidal ideation. Reports mild nausea as side effect.
O (Objective):
- Appearance: Well-groomed, appropriate eye contact
- Affect: Brighter compared to last visit
- Speech: Normal rate and rhythm
- Thought process: Linear and goal-directed
- PHQ-9 score: 8 (down from 18 at last visit)
A (Assessment): Major Depressive Disorder, single episode, moderate, showing improvement with current treatment. Patient is responding well to fluoxetine with significant reduction in depressive symptoms. Mild gastrointestinal side effects present but not severely impacting functioning.
P (Plan):
- Continue fluoxetine 20mg daily; discuss potential for dose increase if residual symptoms persist.
- Provide psychoeducation on managing SSRI side effects.
- Encourage continuation of weekly psychotherapy sessions.
- Order basic metabolic panel and liver function tests to monitor for any abnormalities.
- Discuss sleep hygiene techniques for early morning awakening.
- Follow-up in 4 weeks to reassess symptoms and medication efficacy.
8. Child Therapy SOAP Note Example and Template
Working with children in therapeutic settings requires a unique approach. SOAP notes for child therapy should incorporate both the child's verbal and non-verbal communication styles, as well as observations of their interactions with caregivers or peers. Below is an example to guide you on how to structure a SOAP note for a child therapy session effectively.
Subjective (S): The client, a 6-year-old boy, expressed feelings of sadness about school, saying, "I don't like going to school because the other kids are mean to me." His mother added that he has become more withdrawn over the past few weeks.
Objective (O): During the session, the child appeared anxious and avoided eye contact. He engaged minimally in play activities and displayed fidgeting behaviors. He demonstrated limited interactions with his mother, often responding with monosyllabic answers.
Assessment (A): The child shows signs of social anxiety and possible bullying at school, contributing to his withdrawal and feelings of sadness. These behaviors align with generalized anxiety disorder (GAD) and possible adjustment disorder.
Plan (P):
- Continue weekly individual therapy to build rapport and address anxiety symptoms.
- Implement play therapy techniques to encourage expression and coping skills development.
- Schedule a family session to incorporate parental support and strategies for improving school experiences.
- Coordinate with school personnel to address any bullying incidents and ensure a supportive environment for the child.
- Introduce relaxation exercises and coping strategies appropriate for the child's developmental level.
9. Occupational Therapy SOAP Note Example and Template
Occupational therapists frequently rely on SOAP notes to document patient progress accurately and effectively. Here's a precise example:
Subjective (S): "I'm feeling more comfortable using my left hand for daily activities but still struggle with fine motor tasks," reported Mr. Smith.
Objective (O): During the session, Mr. Smith was able to successfully complete 3 out of 5 buttoning exercises using his left hand within 10 minutes, demonstrating improved dexterity and confidence. However, he experienced difficulty with more delicate tasks such as threading a needle.
Assessment (A): Mr. Smith is showing significant improvement in gross motor skills with his left hand but continues to face challenges with fine motor tasks. The progress aligns with the goal of regaining basic hand functionality, indicating positive development. However, further focus on fine motor activities is necessary.
Plan (P): Continue the current therapy regimen focusing on gross motor skills while incorporating additional fine motor exercises such as threading beads and practicing handwriting. Reassess progress in the next session and modify the plan as needed based on Mr. Smith's improvement.
This detailed approach in documenting SOAP notes not only ensures accurate records but also aids in tailoring specific therapeutic interventions to meet the patient's evolving needs.
10. Speech Therapy SOAP Note Example and Template
Speech therapy notes look similar in many ways to occupational therapy notes, with a focus on speech.
Date: September 20, 2023
Subjective (S): The patient, a 7-year-old male, reports feeling frustrated when trying to communicate with peers at school. The patient's mother also notes that he seems to avoid social interactions, possibly due to his speech difficulties.
Objective (O): During the session, the patient demonstrated difficulty with the articulation of /r/ and /s/ sounds. Utilized both structured activities and spontaneous conversation to elicit these sounds. The patient required prompts in 80% of the attempts to correct these articulations.
Assessment (A): The patient's speech impediments are impacting his social interactions and self-esteem. Progress is noted in the production of correct sounds with prompting. Potential underlying issues include phonological processing delays, which should be further evaluated.
Plan (P): Continue targeting /r/ and /s/ sounds in upcoming sessions, utilizing a combination of play-based and structured activities. Incorporate phonological awareness exercises and provide the mother with home practice materials. Reevaluate progress in one month to adjust the treatment plan if necessary.
11. Art Therapy SOAP Note Example and Template
Art therapy offers a unique and profound way to help individuals explore their emotions and experiences through creative expression. SOAP notes for art therapy can capture the subtleties and breakthroughs that occur in these sessions.
Subjective (S): The client expressed feelings of sadness and frustration, describing their week as 'overwhelming.' They mentioned that engaging in the art activities has been a helpful outlet."
Objective (O): The client chose to work with watercolors, creating abstract shapes. They appeared calm and focused throughout the session, with consistent body language reflecting engagement."
Assessment (A): The client's choice of watercolors and abstract forms suggests a desire to manage emotions non-verbally. Their engagement and calm demeanor indicate progress in using art as a therapeutic tool."
Plan (P): Continue to explore various art mediums to help the client find the most effective form of expression. Introduce structured art activities to target specific emotional challenges."
12. CBT SOAP Note Example and Template
CBT sessions are usually much more actionable and tend to be more factual/ include some data.
Subjective (S): The client reports feeling more anxious and experiencing increased intrusive thoughts over the past week. They mention that their sleep has been disturbed and they have been feeling more irritable at work. The client rates their anxiety level as 7 out of 10.
Objective (O): The client appeared visibly anxious during the session, frequently fidgeting and struggling to maintain eye contact. Their speech was fast-paced, and they seemed to be have difficulty in focusing on the conversation. The client was punctual and dressed appropriately, indicating self-care remains intact.
Assessment (A): The client's anxiety levels appear to be elevated compared to the previous sessions. The increase in intrusive thoughts and disturbances in sleep suggest a potential exacerbation of their anxiety disorder. Cognitive distortions, specifically catastrophizing, were evident during the session.
Plan (P): Continue with cognitive behavioral therapy, focusing on cognitive restructuring techniques to address cognitive distortions. Scheduled a follow-up session for next week. Plan to introduce relaxation techniques and sleep hygiene education to manage anxiety symptoms better.
13. Play Therapy SOAP Note Example and Template
Play Therapy is a unique modality that is highly valuable in understanding children who may not be as articulate as adults. The SOAP note here tends to look observational.
Subjective (S): The child expressed feeling worried about school and reluctant to participate in certain activities. They mentioned feeling scared during interactions with peers and described having nightmares frequently.
Objective (O): Observed the child engaging in solitary play with minimal interaction with provided toys. Displayed signs of anxiety, such as fidgeting and avoidance of eye contact. Noted increased tension when discussing school-related topics.
Assessment (A): The child exhibits signs of anxiety, particularly in social situations and school environments. Nightmares and reluctance to engage with peers are consistent with reported fear and anxiety. These symptoms could be impacting the child's overall social development and daily functioning.
Plan (P): Continue to encourage the child to express their feelings through play. Introduce activities aimed at building social skills in a safe environment. Incorporate relaxation techniques such as deep breathing to help manage anxiety. Schedule a follow-up session to monitor progress and adjust interventions as needed.
14. Bipolar Disorder SOAP Note Example and Template
Subjective (S): Client reports increased energy, decreased need for sleep, and engaging in risky behaviors over the past week. States, "I feel like I can do anything."
Objective (O): Client exhibited pressured speech and psychomotor agitation. Dressed flamboyantly and spoke about grandiose plans. Mood appeared euphoric.
Assessment (A): Current presentation consistent with Bipolar I Disorder, current episode manic. Risk of impulsive behavior and poor decision-making elevated.
Plan (P): Urgent referral to psychiatrist for medication adjustment. Discuss importance of sleep hygiene and maintaining routine. Develop safety plan to manage impulsive urges. Schedule more frequent check-ins over the next week.
15. Eating Disorder SOAP Note Template and Example
Subjective (S): Client reports increased restriction of food intake and intense fear of gaining weight. States, "I feel fat even though everyone tells me I'm too thin."
Objective (O): Client appeared significantly underweight. Avoided discussing specific eating habits. Became defensive when topic of weight was broached.
Assessment (A): Symptoms consistent with Anorexia Nervosa, restricting type. Body image distortion evident. Medical complications possible due to low weight.
Plan (P): Coordinate care with nutritionist and primary care physician. Introduce cognitive restructuring to address distorted body image. Discuss potential for higher level of care if weight continues to decrease. Weekly weigh-ins and food journal assignments.
16. OCD SOAP Note Template and Example
Subjective (S): Client reports increasing intrusive thoughts about contamination and spending over 3 hours daily on cleaning rituals. States, "I can't stop thinking about germs everywhere."
Objective (O): Client appeared anxious and had chapped hands from frequent washing. Hesitated to touch objects in the office. Completed Y-BOCS with score indicating severe OCD symptoms.
Assessment (A): Obsessive-Compulsive Disorder with predominant contamination obsessions and cleaning compulsions. Symptoms causing significant distress and impairment in daily functioning.
Plan (P): Continue Exposure and Response Prevention (ERP) therapy. Develop hierarchy of exposures related to contamination fears. Discuss potential benefits of adding medication to treatment plan. Provide psychoeducation about OCD to family members.
17. Crisis Intervention SOAP Note Example and Templare
Subjective (S): Client brought to ER by police after threatening self-harm. States, "I can't take it anymore. I just want to end it all."
Objective (O): Client appeared agitated and tearful. Vital signs appear normal. Physical exam findings reveal superficial cuts on arms. Actively expressed suicidal ideation with plan to overdose on medication.
Assessment (A): Acute suicidal crisis. Major Depressive Disorder with current severe episode. High risk for self-harm.
Plan (P): Recommend inpatient psychiatric admission for safety and stabilization. Conduct thorough risk assessment. Develop safety plan with client and family. Arrange for follow-up outpatient care upon discharge.
18. Schizophrenia SOAP Note Example
Subjective (S): Client reports hearing voices telling them they are being watched. States, "I think my neighbors are spying on me through my TV."
Objective (O): Client appeared disheveled and exhibited disorganized speech. Frequently looked around the room as if responding to internal stimuli. Affect was blunted.
Assessment (A): Symptoms consistent with Schizophrenia, paranoid type. Active auditory hallucinations and paranoid delusions present.
Plan (P): Review medication compliance and efficacy. Introduce reality testing techniques. Discuss coping strategies for managing hallucinations. Coordinate with case manager to ensure stable housing and community support.
Common Mistakes to Avoid When Writing Effective SOAP Notes
To ensure your SOAP notes are effective, avoid these common pitfalls:
- Not Being Specific Enough: Provide detailed information about the client's issues and feelings.
- Leaving out Important Details: Capture key elements of each session, including mood, affect, and interventions used.
- Failing to Record the Client's Direct Quotes: When possible, use the client's exact words for valuable context.
- Missing the "So What?": Analyze themes, assess progress, and reflect your clinical reasoning.
FAQs
Q. Do SOAP notes need to be written in a particular format?
A. SOAP notes should follow a consistent format, but you can adapt it to suit your needs. Clarity and consistency are key.
Q. Should I use whole sentences or bullet points?
A. Either is acceptable. Many clinicians use a combination based on the section. Whole sentences work well for narrative elements, while bullet points enhance readability in objective and plan sections.
Q. What tense should I write in?
A. Use past tense for subjective and objective sections, present tense for assessment, and future or imperative form for the plan. Consistent tense usage improves clarity across your documentation.
Q. How should I organize each section?
A. Present information chronologically or by importance in the Subjective and Objective sections. Organize Assessment by diagnosis or issue priority, and structure Plan by intervention type or timeline.
Q. What if a session runs long or short?
A. Document based on content complexity, not session duration. Focus on clinically relevant information regardless of how long the appointment lasted.
Q. Do I still need a SOAP note if nothing significant happened?
A. Yes. Briefly document topics discussed, current status, and any recommendations made. Even "maintenance" notes establish continuity of care and may reveal patterns over time.
Q. Do I need to use medical terminology?
A. Use terminology you and other providers understand. Explain complex terms or abbreviations. Clinical terms are appropriate when accurate, but avoid unnecessary jargon that might confuse other providers or patients.
Q. What if I make a mistake?
A. For paper records, draw a single line through errors, initial and date the correction, then add correct information. For electronic records, follow your system's amendment process that preserves the original entry.
Q. What if I don't have much for the objective section?
A. Include whatever observable data you can, even if minimal. Note the client's presentation, affect, or body language, and never completely omit this section.
Q. How do I handle sensitive information?
A. Include only clinically relevant information. Use neutral, factual language. Follow your organization's protocols for information requiring additional privacy protections.
Q. Can I use SOAP notes for group therapy?
A. Yes. Summarize group themes in Subjective, capture group dynamics in Objective, address group progress in Assessment, and outline future interventions in Plan. Individual contributions can be noted where significant.
Q. How do I document client progress over time?
A. Reference previous notes, mention changes in symptoms or behaviors, use objective measures, and compare current status to treatment goals. This creates a clear narrative of the treatment journey.
Q. What if a client requests to see their SOAP notes?
A. Review notes first to ensure professional content, be prepared to explain clinical terminology, and consider discussing content verbally to provide context. Follow your organization's policies regarding record release.
Q. How do I handle disagreements about session content?
A. Document both perspectives clearly using attributive phrases like "Client reports..." and "Therapist observed..." without suggesting either is incorrect. Maintain a respectful, non-judgmental tone throughout.
Q. How detailed should the Plan section be?
A. Include enough detail to guide future treatment while remaining adaptable to changing circumstances. Specify short-term goals, interventions, homework, referrals, and follow-up timeframes.
Q. How do I incorporate cultural considerations?
A. Integrate cultural factors throughout all sections where relevant, noting culturally-specific expressions of symptoms, variations in presentation, and culturally appropriate interventions. Avoid assumptions and document the individual's unique cultural identity as it relates to treatment.
Q. Can I use SOAP notes for telehealth sessions?
A. Yes. Follow the same SOAP format while noting the virtual delivery method. Document observable data from video interactions and any environmental factors visible during the session.
Q. How do I handle multiple issues in one SOAP note?
A. Use subheadings within each SOAP section or prioritize the primary concern while briefly addressing secondary issues in the Plan section. Ensure all significant problems are documented appropriately.
Q. How do I ensure continuity with multiple providers?
A. Use a standardized SOAP format that other clinicians can easily follow. Reference previous providers' notes when relevant and ensure all documentation is accessible through shared electronic records when possible.
Recap
Q. What does SOAP stand for?
A. SOAP is a medical note format that stands for Subjective, Objective, Assessment, and Plan. This structured approach to medical documentation helps healthcare providers create comprehensive notes that capture patient experiences, clinical observations, professional analyses, and treatment strategies.
Q. What is the format of a SOAP note?
A. A SOAP note format consists of four clearly labeled sections (Subjective, Objective, Assessment, and Plan) that follow a logical progression. The format should provide sufficient detail for continuity of care while remaining concise and focused on relevant clinical information.
Q. What are the four parts of a SOAP note?
A. The four parts are Subjective (patient's self-reported symptoms and experiences, chief complaint), Objective (observable data and clinical findings), Assessment (professional analysis and diagnostic impressions), and Plan (treatment approach and follow-up details). Each section serves a distinct purpose in creating a complete clinical picture.
Cut Note-Taking Time by 70%
Create HIPAA-compliant drafts in seconds — finish notes before your next client walks in.
Start Free Trial