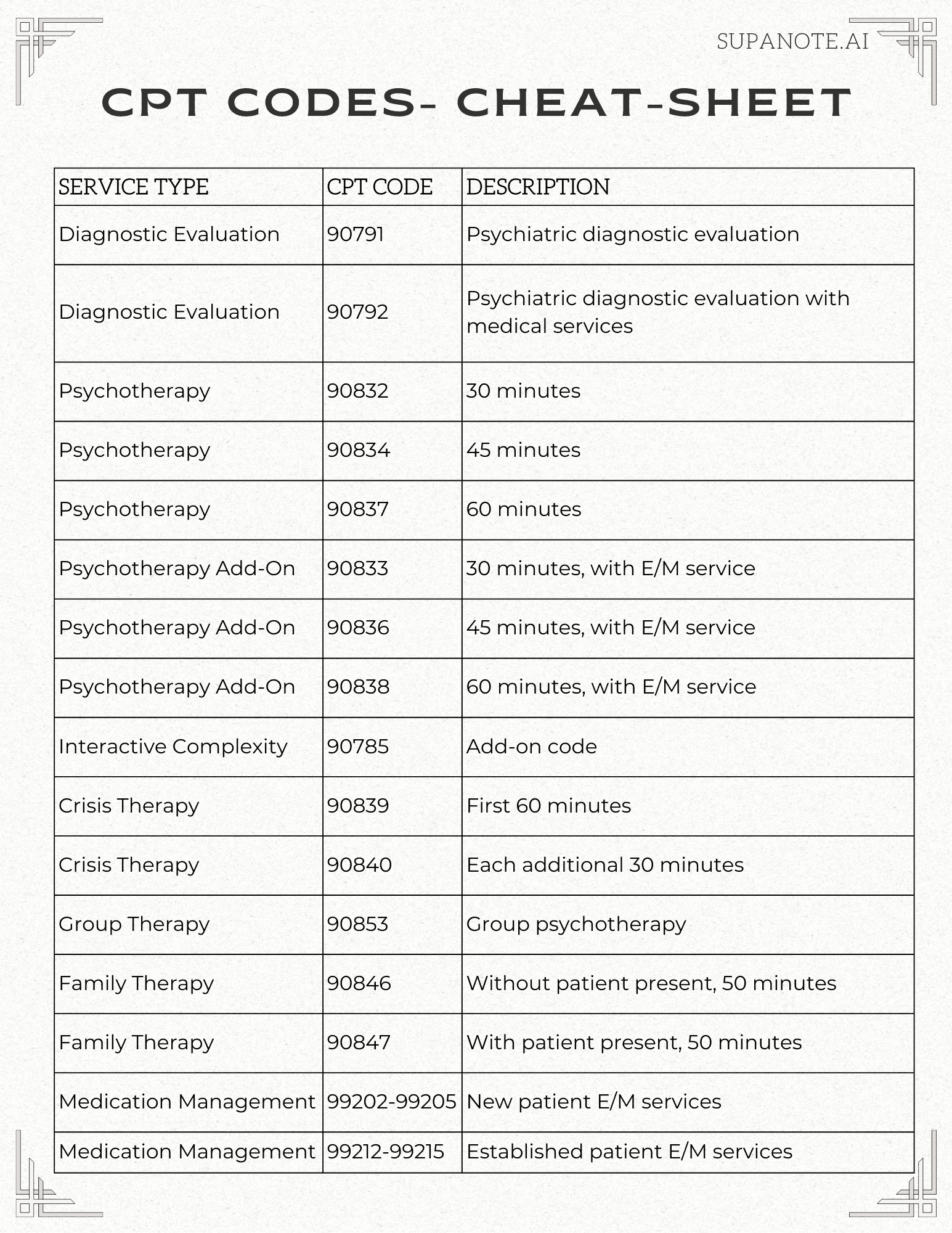
Top CPT Codes: Cheat Sheet and Examples
CHEAT SHEET
Introduction
Current Procedural Terminology (CPT) codes are crucial for psychiatric and psychology practices to accurately bill for services provided. This comprehensive guide will help you navigate the complexities of CPT codes, ensuring proper reimbursement and compliance with billing regulations.
Understanding CPT Codes
Mental health CPT codes, developed by the American Medical Association (AMA), are used to describe medical, surgical, and diagnostic services. In psychiatry, these codes cover a wide range of services, including:
Diagnostic evaluations
Psychotherapy sessions
Medication management
Crisis interventions
Group therapy
Psychological testing
Key Categories of CPT Codes
1. Psychiatric Diagnostic Evaluations
90791: Psychiatric diagnostic evaluation
90792: Psychiatric diagnostic evaluation with medical services
These codes are used for initial evaluations and assessments. They can typically be billed once per episode of illness.
2. Psychotherapy
90832: Psychotherapy, 30 minutes
90834: Psychotherapy, 45 minutes
90837: Psychotherapy, 60 minutes
These codes are used for individual psychotherapy sessions. The time includes face-to-face time with the patient and/or family member.
3. Psychotherapy Add-On Codes
90833: Psychotherapy, 30 minutes, with E/M service
90836: Psychotherapy, 45 minutes, with E/M service
90838: Psychotherapy, 60 minutes, with E/M service
These codes are used when psychotherapy is provided in addition to evaluation and management (E/M) services.
4. Interactive Complexity Add-On Code
90785: Interactive complexity (list separately in addition to the code for primary procedure)
This add-on code is used when there are communication factors that complicate the delivery of a psychiatric procedure.
5. Crisis Therapy
90839: Psychotherapy for crisis, first 60 minutes
90840: Psychotherapy for crisis, each additional 30 minutes
These codes are used for immediate crisis intervention services.
6. Group Psychotherapy
90853: Group psychotherapy (other than of a multiple-family group)
This code is used for group therapy sessions, not including multiple-family group therapy.
7. Family Psychotherapy
90846: Family psychotherapy (without the patient present), 50 minutes
90847: Family psychotherapy (conjoint psychotherapy) (with patient present), 50 minutes
These codes are used for family therapy sessions, with or without the patient present.
8. Medication Management
99202-99205: New patient E/M services
99212-99215: Established patient E/M services
These codes are used for medication management visits, which often involve evaluation and management services.
Best Practices for Using CPT Codes
Accurate Documentation: Ensure your clinical notes support the CPT code billed.
Time Tracking: For time-based codes, document the exact time spent with the patient.
Use an AI scribe to ensure quality of documentation: AI Therapy Note tools like Supanote.ai can write accurate clinical notes for you and ensure they're insurance-compliant
Proper Use of Add-On Codes: Only use add-on codes in conjunction with appropriate primary codes.
Regular Updates: Stay informed about annual updates to CPT codes and descriptions.
Compliance: Familiarize yourself with payer-specific guidelines and compliance requirements.
Audit Readiness: Regularly audit your coding practices to ensure accuracy and compliance.
Common Coding Challenges and Solutions
Challenge: Distinguishing between psychotherapy and E/M services.
Solution: Clearly document the nature of the service provided. If both are provided, use the appropriate psychotherapy add-on code with the E/M code.Challenge: Correctly coding for crisis interventions.
Solution: Use crisis codes (90839, 90840) only for immediate crisis intervention. Document the nature of the crisis and interventions provided.Challenge: Proper use of the interactive complexity add-on code.
Solution: Only use 90785 when specific communication factors complicate delivery of the primary service. Document these factors clearly.Challenge: Coding for extended sessions.
Solution: Use the appropriate time-based code that most closely matches the session duration. Document the exact time spent.Challenge: Billing for multidisciplinary treatments.
Solution: Ensure each provider bills separately for their specific services. Coordinate to avoid duplicate billing.
Comparative Analysis: Mental health CPT Codes vs. Other Medical Specialties
While CPT codes are used across all medical specialties, mental health CPT codes have some unique aspects:
Time-based codes: Mental health codes are typically time-based, unlike procedure-based codes in surgical specialties.
Evaluation and Management (E/M) crossover: Mental health practitioners often use E/M codes, similar to primary care, but with mental health-specific considerations.
Complexity of services: Codes often need to account for the complex nature of mental health treatment, including factors like interactive complexity.
Limited physical procedures: Unlike specialties such as cardiology or orthopedics there are fewer codes for physical procedures.
Emphasis on counseling: Codes reflect the significant role of psychotherapy and counseling in treatment.
Understanding these differences can help in interactions with other specialists and in explaining the nature of psychiatric services to payers and administrators.
Case Studies: Coding Complex Patient Scenarios
Let's explore some real-world scenarios to illustrate proper coding practices: across psychiatry and psychology
Case 1: Initial Evaluation with Medication Management
Scenario: A new patient presents for an initial evaluation. The psychiatrist spends 50 minutes conducting a comprehensive psychiatric evaluation and 25 minutes on medication management.
Coding:
90792 (Psychiatric diagnostic evaluation with medical services)
No separate E/M code, as it's included in 90792
Case 2: Psychotherapy with Medication Adjustment
Scenario: An established patient has a 45-minute psychotherapy session. The psychiatrist also spends 15 minutes on medication management.
Coding:
99214 (Established patient E/M service, moderate complexity)
90836 (Psychotherapy, 45 minutes, with E/M service)
Case 3: Family Therapy with Interactive Complexity
Scenario: A 50-minute family therapy session with the patient present. The patient is a child with autism, requiring significant effort to communicate effectively.
Coding:
90847 (Family psychotherapy with patient present, 50 minutes)
90785 (Interactive complexity add-on)
Telemedicine Coding
With the growing prevalence of teletherapy/ telepsychiatry, understanding how to code for these services is essential:
Place of Service (POS) code: Use POS 02 for telehealth services.
Modifiers:
Modifier 95: Synchronous telemedicine service
Modifier GT: Via interactive audio and video telecommunications systems
Eligible services: Most psychiatric services, including evaluation, psychotherapy, and medication management, can be provided via telehealth.
Time-based coding: The same time-based codes apply to telehealth as in-person services.
Documentation: Clearly document that the service was provided via telehealth, including the patient's location.
State regulations: Be aware of state-specific telehealth laws and regulations, which can affect coding and reimbursement.
State-Specific Regulations in Coding
While CPT codes are standardized nationally, state regulations can impact their use:
Scope of practice: Some states may restrict certain services to specific provider types, affecting who can bill for certain codes.
Telehealth laws: State laws vary regarding the provision and coding of telehealth services.
Medicaid variations: State Medicaid programs may have unique coding requirements or limitations.
Incident-to billing: Rules for incident-to billing can vary by state, affecting how services provided by non-physician practitioners are coded.
Supervision requirements: Some states have specific supervision requirements for certain psychiatric services, which can impact coding.
Always consult your state's specific regulations and guidelines when implementing coding practices.
Coding for Special Populations
Different patient populations may require special coding considerations:
Children and Adolescents
Use of family therapy codes (90846, 90847) is often more frequent.
Play therapy may be coded as psychotherapy, but document techniques used.
School consultations may be billable in some cases (use 99368 for non-face-to-face time).
Elderly Patients
Consider cognitive assessment codes (96116, 96132) for dementia evaluations.
Be aware of Medicare's specific documentation requirements for psychiatric services.
Medication management may be more complex, potentially justifying higher-level E/M codes.
Substance Use Disorders
Use specific codes for substance use assessments (H0001) and interventions (H0004).
Be familiar with codes for intensive outpatient programs (H0015) and partial hospitalization (H0035).
Medication-assisted treatment has specific coding requirements (e.g., G2067 for methadone treatment).
Technology and Coding
The integration of technology in practice impacts coding in several ways:
Electronic Health Records (EHRs): Many EHRs have built-in coding assistance, but it's crucial to verify their accuracy and stay updated on code changes.
AI scribes: AI Scribes like Supanote.ai are a new class of tools from 2024, that can automatically generate your documentation in an insurance-approved manner
Common Audit Findings
Understanding common audit findings can help practices proactively address potential issues and maintain compliance. Here are some typical problems identified during psychiatry coding audits and strategies to avoid them:
1. Insufficient Documentation
Finding: The documentation doesn't support the level of service billed.
Prevention:
Use AI scribes to snsure comprehensive and detailed clinical notes for each session.
Clearly document the time spent and specific services provided.
Use checklists to ensure all necessary elements are included in documentation.
2. Improper Use of Time-Based Codes
Finding: Time-based codes are used without proper time documentation.
Prevention:
Always document the exact start and end times for sessions.
Ensure the time spent meets the minimum requirements for the code used.
Be clear about how time was spent (e.g., face-to-face with patient, coordinating care).
3. Incorrect Use of Add-On Codes
Finding: Add-on codes are billed without the appropriate primary code.
Prevention:
Double-check that the primary code is included when billing add-on codes.
Understand which add-on codes can be used with which primary codes.
Implement a system to flag inappropriate code combinations before billing.
4. Overuse of High-Level E/M Codes
Finding: Consistently billing high-level E/M codes without sufficient justification.
Prevention:
Ensure the complexity of medical decision-making or time spent counseling supports the E/M level.
Regularly audit your own E/M code distribution to identify potential overuse.
Document clearly why a higher-level code was chosen.
5. Lack of Medical Necessity
Finding: Services billed don't meet medical necessity criteria.
Prevention:
Clearly document the patient's diagnosis and how each service relates to treating that diagnosis.
Regularly update treatment plans to reflect ongoing medical necessity.
Be familiar with payer-specific medical necessity requirements.
6. Improper Use of Psychotherapy Add-On Codes with E/M Services
Finding: Psychotherapy add-on codes used with E/M services without clear delineation of services.
Prevention:
Clearly document both the E/M component and the separate psychotherapy component of the visit.
Ensure the time spent on psychotherapy meets the minimum requirements for the add-on code.
Be prepared to demonstrate that psychotherapy was a significant, separately identifiable service.
7. Incorrect Coding for Group vs. Individual Therapy
Finding: Individual therapy codes used for group sessions or vice versa.
Prevention:
Use the appropriate code for the type of therapy provided (e.g., 90853 for group therapy).
If both individual and group therapy are provided on the same day, document each service separately.
Be clear about the number of participants in group sessions.
8. Upcoding Interactive Complexity
Finding: Overuse or improper use of the interactive complexity add-on code (90785).
Prevention:
Only use 90785 when specific factors complicate the delivery of the primary psychiatric procedure.
Clearly document the factors that justify the use of this add-on code.
Be familiar with the specific criteria for interactive complexity.
9. Inappropriate Use of Prolonged Service Codes
Finding: Prolonged service codes used without meeting time thresholds or proper documentation.
Prevention:
Only use prolonged service codes when time spent significantly exceeds typical service time.
Document start and end times for the entire service, including prolonged time.
Be familiar with the specific time thresholds required for prolonged service codes.
10. Failure to Update Diagnoses
Finding: Outdated or inaccurate diagnosis codes used in billing.
Prevention:
Regularly review and update patient diagnoses.
Ensure each claim includes the most current and accurate diagnosis codes.
Implement a system to flag outdated diagnoses in patient records.
Frequently Asked Questions (FAQs)
To further assist you in understanding and applying Psychiatry CPT codes, here are answers to some frequently asked questions:
Q: What's the difference between 90791 and 90792?
A: Both are used for initial psychiatric evaluations. 90791 is for a diagnostic evaluation without medical services, while 90792 includes medical services such as prescribing medications.
Q: Can I bill for time spent on documentation?
A: Generally, no. CPT codes typically cover face-to-face time with the patient. However, some non-face-to-face services like care coordination may be billable under specific circumstances.
Q: How do I code for a session that runs longer than the standard time?
A: Use the CPT code that most closely matches the actual time spent. For significantly extended sessions, consider using the appropriate prolonged service code.
Q: Can I use psychotherapy codes (90832, 90834, 90837) and E/M codes (99xxx) on the same day?
A: Generally, you should use the appropriate E/M code with a psychotherapy add-on code (90833, 90836, 90838) rather than billing both separately.
Q: How often can I bill for a psychiatric diagnostic evaluation (90791 or 90792)?
A: Typically, these are used for initial evaluations. Some payers may allow their use for re-evaluations, but frequency is often limited. Check with specific payers for their policies.
Q: What documentation is needed to support the use of the interactive complexity add-on code (90785)?
A: You should document the specific factors that complicated the delivery of the primary service, such as the need to manage maladaptive communication or the involvement of third parties.
Q: How do I code for medication management without psychotherapy?
A: Use the appropriate E/M code (99212-99215 for established patients) based on the complexity of the visit or time spent.
Q: Can multiple providers bill for services provided to the same patient on the same day?
A: This depends on the specific services and payer policies. In many cases, it's allowable if the services are distinct, but clear documentation is crucial.
Q: How do I code for a family therapy session where the patient is present for only part of the session?
A: Use 90847 (family psychotherapy with patient present) if the patient is present for any part of the session. Document the time the patient was present and absent.
Q: Are there any special considerations for coding geriatric psychiatry services?
A: While the basic CPT codes remain the same, be aware of Medicare's specific documentation requirements. Also, consider using cognitive assessment codes (e.g., 96116) when appropriate.
Q: How do I code for telepsychiatry sessions?
A: Use the same CPT codes as you would for in-person visits, but add the appropriate telehealth modifier (usually 95 or GT) and use the correct Place of Service code (typically 02 for telehealth).
Q: Can I use psychotherapy codes for sessions focused primarily on medication management?
A: If the session is primarily for medication management, it's more appropriate to use E/M codes. Psychotherapy codes should only be used when a significant amount of psychotherapy is provided.
Q: How do I code for group therapy sessions of varying lengths?
A: The group therapy code 90853 is not time-specific. Use this code regardless of the session length, but document the actual time spent.
Q: What's the difference between using an E/M code with a psychotherapy add-on versus just using a psychotherapy code?
A: Use an E/M code with a psychotherapy add-on when you provide both medical evaluation/management and psychotherapy in the same session. Use a standalone psychotherapy code when the session is purely psychotherapy without significant medical management.
Q: How do I code for crisis intervention services?
A: Use 90839 for the first 60 minutes of psychotherapy for crisis, and 90840 for each additional 30 minutes. These codes are used for immediate crisis intervention services.
Q: Can CPT code 90839 (crisis) be used with 90837 ?
A: No, CPT codes 90839 and 90837 should not be used together for the same session. These codes are mutually exclusive as they represent different types of services:
90837 is used for a standard 60-minute psychotherapy session.
90839 is specifically for the first 60 minutes of psychotherapy for crisis.
If a crisis intervention extends beyond 60 minutes, you would use 90839 for the first 60 minutes and 90840 for each additional 30 minutes. The key difference is that 90839 is specifically for crisis intervention, which is distinct from a regular psychotherapy session (90837). It's important to note that crisis intervention (90839) implies an urgent assessment and history of a crisis state, a mental status exam, and a disposition. This is different from a standard psychotherapy session, even if that session deals with a patient in a distressed state. Always remember to document clearly the nature of the crisis and the interventions provided to support the use of the crisis code.
Psychiatry CPT Codes Cheat Sheet
Here's a quick reference guide for the most common CPT codes:
References and Further Reading
For more information on Psychiatry CPT codes and related topics, please refer to the following resources:
American Medical Association (AMA) - CPT® (Current Procedural Terminology): https://www.ama-assn.org/practice-management/cpt
Centers for Medicare & Medicaid Services (CMS) - Mental Health Services: https://www.cms.gov/medicare-coverage-database/view/ncd.aspx?ncdid=308
National Council for Mental Wellbeing - Billing & Coding Resources: https://www.thenationalcouncil.org/resources/
American Psychological Association (APA) - Documenting and Coding Psychological Services: https://www.apaservices.org/practice/reimbursement/health-codes/documentation
Journal of Clinical Psychiatry - CPT Coding Updates: https://www.psychiatrist.com/