As behavioral health professionals, mastering the Mental Status Exam (MSE) is crucial for providing effective care to your clients. This guide will equip you with the knowledge and tools to conduct thorough MSEs, allowing you to identify certain mental health conditions more easily, and informing your treatment planning.
In this blog, we'll cover the following:
- Key components of a mental status examination
- A guide to conducting each part of the exam with examples and assessment techniques
- A full example of a complete MSE
- Practical challenges and solutions
- Cultural considerations in MSE assessment
If instead you're looking for a comprehensive guide on how to do a biopsychosocial examination, refer to this guide here.
The Purpose of the Mental Status Exam
The Mental Status Exam is a structured assessment of a client's cognitive and emotional functioning at a specific point in time. It serves several crucial purposes:
- Provides a baseline of the client's mental state
- Aids in differential diagnosis
- Helps track changes in symptoms over time
- Informs treatment planning and interventions
- Facilitates communication with other healthcare providers
You'd want to do a brief mental status exam at the beginning of any new client relationship, to identify potential mental health conditions.
Components of the Mental Status Exam
A comprehensive mental status exam typically covers the following 10 components:
- Appearance and Behavior
- Attitude
- Motor Activity
- Speech
- Mood and Affect
- Thought Process
- Thought Content
- Perception
- Cognition
- Insight and Judgment
We cover each of these in depth later in this article.
What is a Mini Mental State Exam?
In contrast to the comprehensive mental status exam (MSE), the "mini" mental state examination (MMSE) is a specific, structured screening tool designed primarily to assess cognitive impairment.
It consists of a series of questions and tasks that focus on orientation, registration, attention and calculation, recall, and language.
While the MSE is used broadly in mental health evaluations, the MMSE is particularly useful for detecting and monitoring cognitive decline, such as in cases of dementia or delirium.
The MSE provides a broader picture of mental functioning, while the MMSE offers a more focused and quantifiable assessment of cognitive abilities.
How to Conduct the Mental Status Exam
1. Appearance and Behavior
In this section, observe and document the following:
- Age, gender, ethnicity
- Attire and grooming
- Posture and eye contact
- Any notable physical characteristics or abnormalities
Typical Example: "35-year-old Caucasian male, appears stated age. Well-groomed, dressed in business casual attire. Makes appropriate eye contact and sits with an open posture."
Atypical Example: "35-year-old Caucasian male, appears older than stated age. Disheveled appearance with stained clothing and strong body odor. Avoids eye contact and sits hunched over with crossed arms."
Assessment Prompts:
- "Can you tell me about your typical daily routine, including how you prepare for the day?"
- "How would you describe your energy levels lately?"
2. Attitude
Assess the client's approach to the interview: Cooperative, guarded, hostile, seductive, etc.
Typical Example: "Client demonstrates a cooperative attitude, readily engaging in the assessment process."
Atypical Example: "Client exhibits a guarded and somewhat hostile attitude, providing minimal responses and frequently challenging the purpose of questions."
Assessment Prompts:
- "How do you feel about being here today?"
- "What are your expectations for our session?"
3. Motor Activity
Note the body language and any unusual movements or behaviors:
- Psychomotor agitation or retardation
- Tics, tremors, or unusual mannerisms
Typical Example: "Client displays normal psychomotor activity, with no unusual movements noted."
Atypical Example: "Client exhibits significant psychomotor agitation, frequently shifting in the seat, tapping feet, and fidgeting with hands."
Assessment Prompts:
- "Have you noticed any changes in your energy levels or ability to sit still recently?"
- "Do you ever experience any involuntary movements or sensations?"
4. Speech
Here we evaluate the client's speech patterns. Look at the following elements -
- Rate: pressured, rapid, normal, slow
- Volume: loud, soft, normal
- Tone: monotone, expressive
- Content: relevant, coherent, tangential
Typical Example: "Speech is of normal rate, volume, and tone. Content is relevant and coherent."
Atypical Example: "Speech is rapid and pressured, with increased volume. Content is tangential, frequently veering off-topic."
Assessment Prompts:
- "How would you describe your typical speaking style?"
- "Have others commented on changes in your speech recently?"
5. Mood and Affect
Here we evaluate a patient's emotional state.
Mood: This is the client's self-reported emotional state. We use the client's subjective descriptions of their emotions.
Affect: This is the observed expression of emotion. Remember the ABCs of Affect:
A - Affect: The outward expression of emotion
B - Behavior: How the emotion is expressed through actions
C - Cognition: The thoughts associated with the emotion
When assessing affect, consider:
- Range: full, restricted, flat
- Intensity: normal, blunted, exaggerated
- Stability: stable, labile
- Appropriateness to content
Typical Example: "Client reports mood as 'pretty good.' Affect is full range, appropriate to content, and congruent with reported mood."
Atypical Example: "Client reports feeling 'numb.' Affect is flat, with minimal facial expression or vocal inflection, incongruent with the emotional content being discussed."
Assessment Prompts:
- "How would you describe your mood over the past week?"
- "On a scale of 1-10, with 10 being the best you've ever felt and 1 being the worst, where would you rate your mood right now?"
- "Have you noticed any changes in your ability to feel pleasure or interest in activities?"
6. Thought Process
Here we evaluate the patient's thought processes, like the flow and organization of thoughts:
- Logical and goal-directed
- Circumstantial
- Tangential
- Flight of ideas
- Loose associations
- Thought blocking
Typical Example: "Thought process is logical and goal-directed, with client able to provide clear and relevant responses."
Atypical Example: "Thought process is tangential, with client frequently going off on unrelated tangents and struggling to return to the original topic."
Assessment Prompts:
- "Can you walk me through your typical day, from morning to night?"
- "How would you describe your ability to concentrate and focus lately?"
7. Thought Content
Here we are assessing for the presence of:
- Delusions
- Obsessions
- Phobias
- Suicidal and homicidal ideation
Typical Example: "No evidence of delusions, obsessions, or phobias. Denies current suicidal or homicidal ideation."
Atypical Example: "Client expresses paranoid delusions, believing that the government is monitoring their thoughts through implanted devices. Reports frequent intrusive thoughts about contamination."
Assessment Prompts:
- "Do you ever have thoughts that you can't seem to get out of your head?"
- "Have you ever felt like others can read your thoughts or control your mind?"
- "Do you ever have thoughts of harming yourself or others?"
8. Perception
Evaluate for any perceptual disturbances:
- Hallucinations (specify type: auditory, visual, tactile, etc.)
- Illusions
- Depersonalization
- Derealization
Typical Example: "No reported or observed perceptual disturbances."
Atypical Example: "Client reports auditory hallucinations of voices commenting on their actions. Also describes episodes of depersonalization, feeling detached from their body."
Assessment Prompts:
- "Have you ever seen, heard, or felt things that others don't seem to experience?"
- "Do you ever feel disconnected from yourself or your surroundings?"
9. Cognition
Here, use the GOAL CRAMP mnemonic:
G - General alertness
O - Orientation (person, place, time, situation)
A - Attention and concentration
L - Language
C - Calculation
R - Right/left orientation
A - Abstraction
M - Memory (immediate, recent, remote)
P - Praxis
Typical Example: "Alert and oriented x4. Attention, concentration, and memory appear intact. Able to perform simple calculations and demonstrate abstract thinking."
Atypical Example: "Oriented to person and place, but confused about time. Attention span is limited, struggling with serial 7s. Recent memory impaired, unable to recall events from earlier in the day."
Assessment Prompts:
- "Can you tell me today's date, including the day, month, and year?"
- "I'm going to say three words. Please repeat them back to me, and try to remember them because I'll ask you to recall them later: Apple, Penny, Table."
- "Can you count backwards from 100 by 7s?"
10. Insight and Judgment
Assess the client's
- Understanding of their condition (insight)
- Decision-making ability (judgment)
Typical Example: "Client demonstrates good insight into their anxiety, recognizing its impact on daily functioning. Judgment appears sound, as evidenced by seeking professional help and adhering to treatment recommendations."
Atypical Example: "Client lacks insight into their manic symptoms, believing increased energy and risky behaviors are signs of improved mental health. Judgment is impaired, as demonstrated by recent impulsive financial decisions."
Assessment Prompts:
- "What do you think might be causing the difficulties you're experiencing?"
- "How do you think these issues are affecting your life?"
- "What steps have you taken to address these problems?"
Example of a Full Mental Status Exam
Here's a comprehensive example of an MSE write-up:
"Jane Doe is a 42-year-old African American female who presented for evaluation of depressive symptoms. She appeared her stated age, was neatly groomed, and dressed appropriately in casual attire. Her eye contact was intermittent, and she displayed psychomotor retardation, moving and speaking slowly.
Jane's attitude was cooperative but guarded. Her speech was soft and slow, with increased latency in responses. She described her mood as "hopeless," and her affect was constricted, predominantly sad, and congruent with reported mood.
Thought process was logical and goal-directed, albeit slow. Thought content revealed passive suicidal ideation without plan or intent, and feelings of worthlessness. She denied hallucinations, delusions, or obsessions.
Jane was alert and oriented x4. Attention and concentration were mildly impaired, struggling with serial 7s but able to spell "WORLD" backwards. Recent memory was intact, recalling 3/3 objects after 5 minutes. Abstract thinking and judgment were fair.
Jane demonstrated good insight into her depression, recognizing the need for treatment. No obvious cognitive deficits were noted during the examination."
Using AI for Mental Status Exam
Today, AI tools can automatically write a high-quality mental status exam. One exciting development in this area is the automation of therapy notes using artificial intelligence, which offers significant time-saving potential for therapists.
Automating MSE notes with Supanote
Supanote is an AI platform that can automatically write mental status exams for you, directly from your sessions, covering all the topics above. Here are some key features and benefits:
- Direct Session Capture: Supanote can listen directly to therapy sessions and automatically generate a high-level MSE based on the conversation.
- Built-in MSE Template: The system comes with a pre-configured MSE note template, ensuring that all generated notes follow the correct format and structure.
- HIPAA Compliance: Supanote is designed to be HIPAA-compliant, providing a high level of security for sensitive patient information. This compliance is crucial for maintaining patient confidentiality and meeting regulatory requirements.
- Time-Saving: By automating the note-taking process, Supanote can potentially save therapists hours of documentation time each week. This allows clinicians to focus more on patient care and less on administrative tasks.
Below is an example of a sample MSE auto-generated by Supanote AI based on a session. You can also edit the template on Supanote to include the specific sections you'd like.
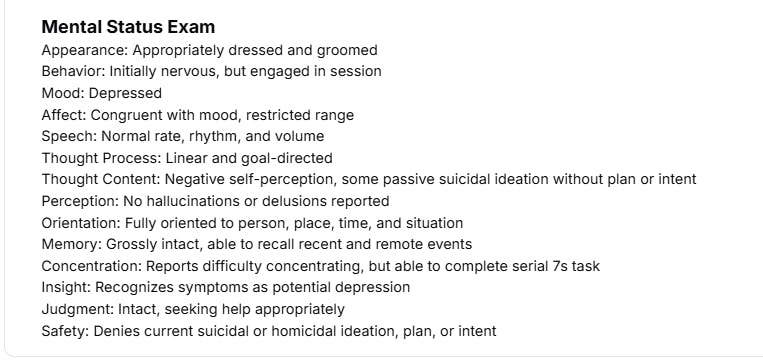
The gap in Supanote and other AI tools is that they don't yet process the visuals - e.g., the patient's facial expressions. So while you will get an MSE, it is best to go through and edit it and update with your own observations (the notes are directly editable).
The MSEs generated by these tools are not intended to be a replacement to your clinical judgement, but as supporting tools to save time for clinicians.
Save 4 Hours Every Week on Notes
Generate HIPAA-compliant drafts in seconds and focus more on your clients, not paperwork.
Start Free Trial
Tips for Conducting an Effective MSE
- Start with open-ended questions to build rapport before moving to more specific inquiries.
- Use natural transitions between topics to cover different aspects of the MSE.
- Pay attention to non-verbal cues throughout the session.
- Practice active listening and reflection to encourage client disclosure.
- Be prepared to pause the assessment if the client becomes distressed or needs a break.
- Document observations in real-time or immediately after the session to ensure accuracy.
- Regularly review and refine your MSE skills through peer consultation and continuing education.
Practical Challenges and Solutions
1. Time Management
Challenge: Conducting a thorough MSE can be time-consuming, especially in busy clinical settings.
Solution: Prioritize key components based on presenting concerns. Integrate MSE questions naturally into the conversation. Use standardized brief cognitive assessments when appropriate.
2. Balancing Standardization and Individualization
Challenge: Adhering strictly to a standardized MSE format may miss important individual nuances.
Solution: Use the standard MSE as a framework, but allow flexibility to explore areas of particular concern for each client. Document any deviations from the standard format and the rationale for them.
3. Building Rapport While Assessing
Challenge: Formal assessment can sometimes feel impersonal or intimidating to clients.
Solution: Explain the purpose of the MSE to clients. Use a conversational tone and integrate assessment questions naturally into the discussion. Pay attention to the client's comfort level and take breaks if needed.
4. Cultural Competence
Challenge: Interpreting MSE findings accurately across diverse cultural backgrounds.
Solution: Continuously educate yourself on cultural differences in mental health presentation. When unsure, ask clients about their cultural background and how it might influence their experiences. Consult with colleagues or cultural experts when needed.
Common Pitfalls to Avoid
- Rushing through the assessment
- Making assumptions based on appearance or initial impressions
- Overlooking subtle signs of cognitive impairment or emotional distress
- Failing to consider cultural factors in interpretation
- Using jargon or technical terms when documenting, rather than clear, descriptive language
Cultural Considerations in MSE Assessment
When conducting an MSE, it's crucial to consider cultural factors that may influence a client's presentation.
Here are some examples:
- Eye Contact: In some Asian and Middle Eastern cultures, direct eye contact with authority figures may be considered disrespectful. A client averting their gaze might be showing respect rather than indicating depression or anxiety.
- Emotional Expression: Some cultures value emotional restraint, while others encourage more open expression. A client from a culture that emphasizes stoicism may appear to have a restricted affect, even when experiencing intense emotions.
- Spiritual Beliefs: In certain African, Native American, or other indigenous cultures, hearing the voice of a deceased relative might be considered a comforting spiritual experience rather than a hallucination.
- Thought Content: Cultural beliefs about spirits, ancestral communication, or supernatural phenomena could be misinterpreted as delusions in a Western context.
- Personal Space: Cultures differ in their norms for personal space. A client who stands very close or far away may be adhering to their cultural norms rather than displaying unusual behavior.
Always strive to understand the client's cultural background and how it might influence their presentation. When in doubt, respectfully ask the client about their cultural practices and beliefs.
Mental Status Exam Template and Cheat Sheets
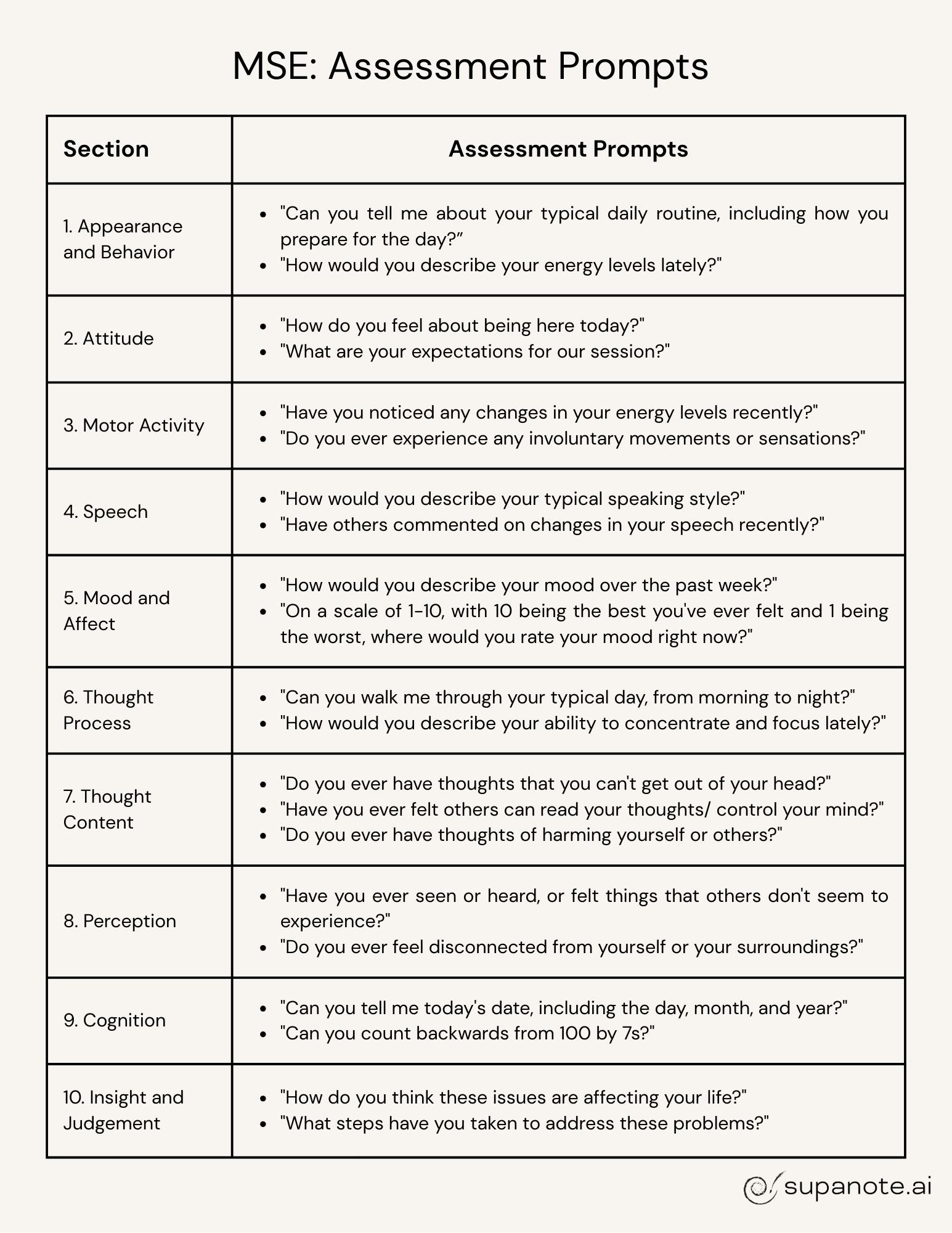
Below is a simple mental status exam cheat sheet you can use to refer to the different components of a mental status exam. It's a reference guide you can look at to make sure you covered all the individual components, and what's expected in each section.
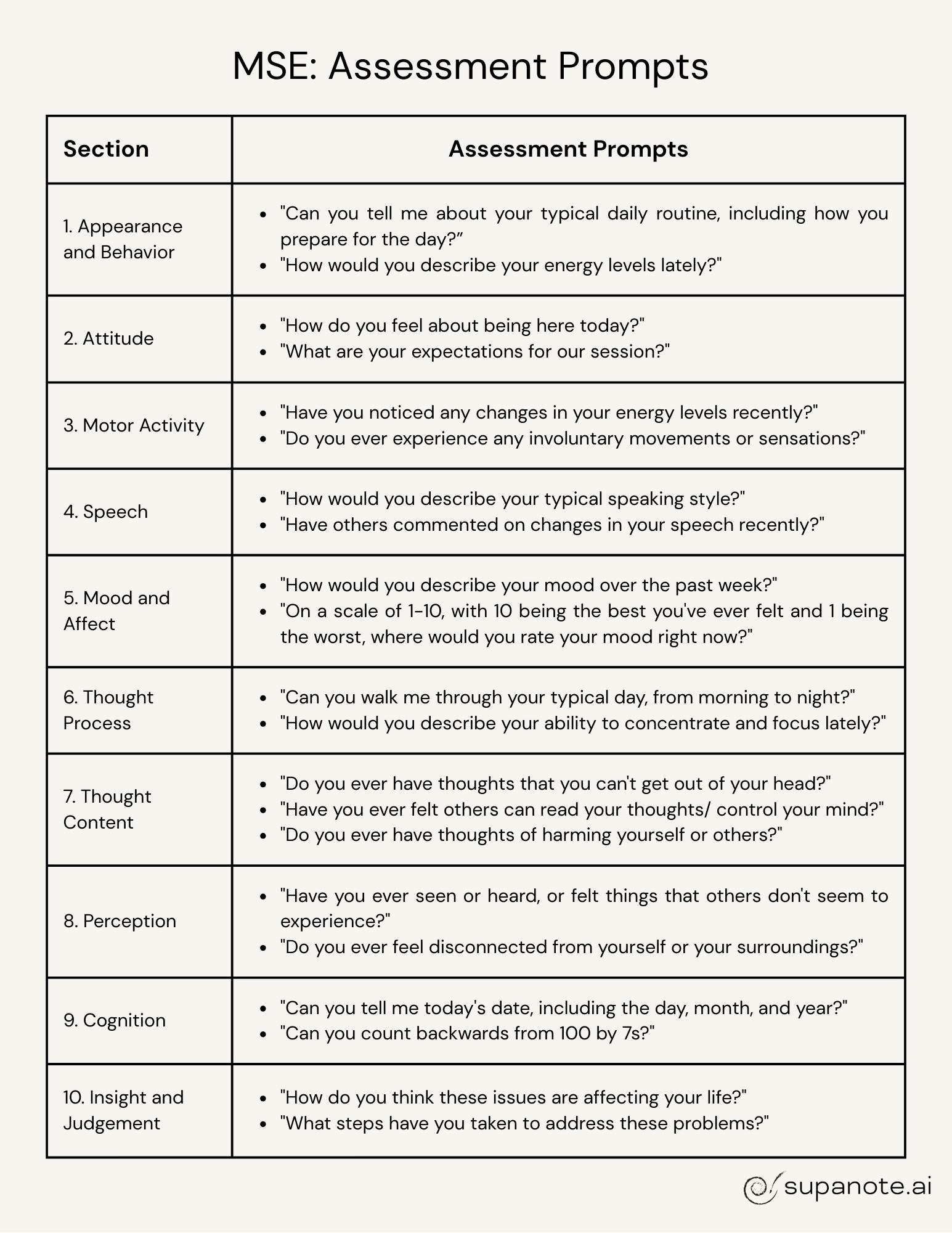
Also see below another cheat sheet with the assessment prompts/ questions you can use for each of the sections
Conclusion
Mastering the Mental Status Exam is an ongoing process that requires practice and refinement. By consistently applying the principles and techniques outlined in this guide, you'll enhance your clinical acumen and provide more targeted, effective care for your clients. Remember, the MSE is not just a checklist but a dynamic tool that, when used skillfully, can provide invaluable insights into your client's mental health and guide your therapeutic interventions.
Keep this cheat sheet handy as a quick reference during your assessments, and don't hesitate to adapt it to your specific practice needs and client populations. With time and experience, conducting a comprehensive MSE will become second nature, allowing you to focus on building strong therapeutic relationships and delivering high-quality mental health care.
FAQs
Here are some common queries about Mental Status Exams
Q. How long should a Mental Status Exam take?
A: Typically, a comprehensive mental status exam takes about 15-30 minutes. But don't sweat it if it takes longer when you're just starting out. With practice, you'll get faster and smoother!
Q. Do I need to cover every component of the mental status exam in every session?
A: Not necessarily. While it's ideal to cover all bases, you can focus on the most relevant areas based on your client's presenting issues. Just make sure to document why you skipped certain parts.
Q. How often should I conduct a mental status exam ?
A: At minimum, do a full MSE during the initial assessment. After that, it's good practice to do brief check-ins each session and a more thorough review periodically or when you notice significant changes.
What if my client refuses to participate in certain parts of the MSE?
A: Respect their boundaries, but document their refusal and any observations you can still make. Try to understand why they're hesitant – it might provide valuable clinical insights.
Q. How do I explain the purpose of an MSE to my clients?
A: Keep it simple and friendly. You might say something like, "I'm going to ask you a few questions to get a clearer picture of how you're doing right now. This helps us understand your current needs better and plan the most effective treatment."
Q. Are there any standardized forms for conducting an MSE?
A: While there's no universally standard form, many clinics and institutions have their own. Check with your workplace or professional association for recommended templates.
Q. How detailed should my MSE notes be?
A: Aim for clear, concise, and objective observations. Use direct quotes when relevant, and always document any safety concerns thoroughly.
Q. Can I use an MSE with children or adolescents?
A: Absolutely! Just adjust your language and expectations to be developmentally appropriate. Play-based assessments can be particularly useful for younger kids.
Q. What if I suspect cognitive impairment during an MSE?
A: If you notice significant cognitive issues, it's a good idea to use more specific cognitive screening tools (like the MMSE or MoCA) and consider referring for neuropsychological testing.
Q. How do I improve my MSE skills?
A: Practice, practice, practice! Conduct MSEs regularly, seek feedback from colleagues, review recorded sessions if possible, and stay updated with continuing education. The more you do it, the more natural it becomes.
Remember, these FAQs are just the tip of the iceberg. Keep asking questions, stay curious, and never stop learning.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. https://www.psychiatry.org/psychiatrists/practice/dsm
- Folstein, M. F., Folstein, S. E., & McHugh, P. R. (1975). "Mini-mental state": A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12(3), 189-198. https://doi.org/10.1016/0022-3956(75)90026-6
- Groth-Marnat, G., & Wright, A. J. (2016). Handbook of psychological assessment (6th ed.). John Wiley & Sons. https://www.wiley.com/en-us/Handbook+of+Psychological+Assessment%2C+6th+Edition-p-9781118960646
- Karasz, A., & Singelis, T. M. (2009). Qualitative and mixed methods research in cross-cultural psychology. Journal of Cross-Cultural Psychology, 40(6), 909-916. https://doi.org/10.1177/0022022109349172
- Kontos, N., Freudenreich, O., & Querques, J. (2016). The mental status examination: A comprehensive approach to its components and performance. Psychiatric Clinics, 39(4), 605-621. https://www.sciencedirect.com/science/article/abs/pii/S0193953X16300399?via%3Dihub
- Morrison, J. (2014). The first interview (4th ed.). Guilford Press. https://www.guilford.com/books/The-First-Interview/James-Morrison/9781462515554
Cut Note-Taking Time by 70%
Create HIPAA-compliant drafts in seconds — finish notes before your next client walks in.
Start Free Trial